Research
Home » Research
Research at the CARE Center
Through research, members of the CARE Center offer solutions to today’s most pressing health issues related to cognitive aging. Our work is collaborative and on the vanguard of aging research. The CARE Center is housed in the Institute of Gerontology, supported by multi-million dollars in grant funding.

Exploring How Carpet Patterns Affect Walking in Older Adults with and without Memory Difficulties
As we age, we experience changes in our abilities to think, see, balance, and navigate from place to place. Those changes are not always considered when flooring choices are made for homes and residential care homes. In this research study, we would like to learn more about how different carpet patterns and colors affect a person’s ability to walk while thinking. Also, we would like to know whether people prefer some colors and patterns to others. Are you interested in participating? See the flyer below for more information!

CARE AwARE (Awareness and Resilience Through Education) Program
Due to the aging US population, health organizations are prioritizing dementia awareness and prevention methods. Improving lifestyle factors may prevent some forms of dementia. Dementia disparities are disproportionately higher in rural areas due, in part, to greater likelihood of dementia-related risk factors. The purpose of this project is to develop and pilot a brain health and dementia risk-reduction program tailored to rural audiences. We offer a variety of topics—like spotting the early signs of dementia and the importance of eating well to help prevent cognitive decline—that are stand alone and fit into existing nutrition and wellness programs. Our team also creates tailored handouts and resource guides to reflect the needs of rural communities.

The CARE Community Dementia Needs Assessment (CDNA)
Alzheimer’s disease and related dementias (ADRD) currently affect 55 million people worldwide and are expected to rise to 78 million by 2030. Rural-dwelling persons in the Southeastern US region have higher ADRD mortality and lower access to preventive, specialty, and allied healthcare, which results in underdiagnosis and a lack of post-diagnosis support services. The purpose of this ongoing needs assessment is to identify community needs around access to ADRD diagnosis, to inform public health programming.

CNA Education
Healthcare facilities face significant staffing shortages despite the increased assistive care needs for a growing aging adult population. Although Certified Nursing Assistants (CNAs) are critical for assistive care, job burnout is high due to physical exhaustion, disproportionally low wages, and disparaging work value. CNAs indicate that skill-building training is a viable retention strategy. The purpose of this project is to design an online CE program using self-care and skill-building to support CNA retention and career sustainability. The University of Georgia and the CNA Career Pathway Initiative (led by UGA Institute of Disaster Management) collaborated with Central Georgia Technical College to develop, distribute, and evaluate an asynchronous CE curriculum for CNAs. Lesson modules are designed to 1) refresh prior knowledge, 2) apply knowledge to client care and skill-building, and 3) incorporate CNA self-care methods to encourage career sustainability.

Extending Outreach to Rural Communities Through Faith Leaders
Faith communities have a long tradition of stepping in where help is needed. Yet, formal partnerships between public health academics and faith communities are rare. In a number of communities, we are working with faith leaders to guide CARE’s outreach programming. The main takeaway is a need to develop a paired approach to training faith-based communities, where faith leaders offer a spiritual underpinning to the evidence-based information the CARE team is best equipped to provide. Continueed work will investigate offering dementia education opportunities offered by rural churches, and equipping churches with the right resources to provide support to their practitioners and families navigating dementia diagnosis and care.

Meet Me At the Gardens
Family caregivers of persons living with dementia experience high mental and physical demand, often creating imbalance and strain within their familial relationships. Research shows exposure to nature (e.g., indoor/outdoor gardens) reduces stress and improves quality of life. In collaboration with the State Botanical Garden, Meet Me at the Garden (MMATG) provides tailored programming for caregiver-patient dyads in a public garden setting. Our initial pilot study has shown that dementia-friendly and informed programming can improve engagement and quality of life for patient-caregiver dyads, particularly when best practices for dementia-informed programming are adopted. Future programming will expand this program in Athens and surrounding rural counties.

Minority Health and Health Disparities
The United States is increasingly diverse. About 40 percent of the population belongs to a racial or ethnic minority group, and by 2060 this percentage is expected to increase to 61 percent. Older minorities suffer disproportionately from a number of negative health outcomes, which is why the Institute of Gerontology is committed to research that may offer solutions to improve health for everyone living in our communities. News story:

Nutrition and Mindfulness
The Mind Your Heart Project addresses how to use mindful eating help individuals maintain a healthy nutritional diet. We offer web-based education on the DASH Diet, combined with mindfulness techniques, that can be completed anytime, anywhere. Our program is a science-based program to help adults make lifelong diet quality changes in a sustainable way
Optics / Vision Science
The primary goal of the Optics and Vision Science research program is to conduct basic and applied studies on the visual system. A primary focus of this program has been the study of the dietary carotenoids lutein and zeaxanthin, concentrated within the fovea (termed macular pigment or the macula lutea) and brain. These studies have ranged across populations, infants to older adults, normal to diseased, and techniques, from pyschophysics to neuroimaging.
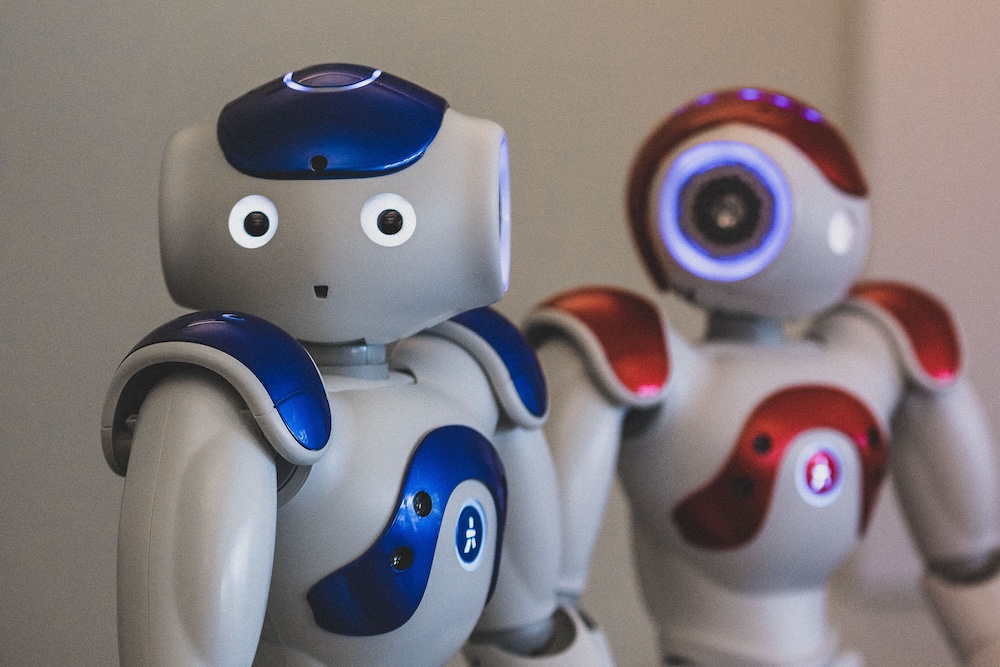
Socially Assistive Robots in Assisted Living Facilities
Socially assistive robots (SAR) can lead healthy enrichment activities and connect assisted living residents to their loved ones, increasing feelings of belonging and potentially improving health behaviors. The purpose of this series of studies is to explore residents, family care partners’ (CP), and assisted living staff perceived benefits and concerns of SAR to provide social engagement. Our preliminary analysis suggest both promise in SAR-enabled health prompts, activity reminders, and trivia as social engagement and health promotion opportunities – however personalization and customization of the technology is key to user acceptance. The assistive nature of SARs is likely needed to adapt to user capability, as residents cognition changes as the disease progresses. News Story:

Social Connectedness
Social connections are integral to human well-being. A lack of social connectedness is associated with morbidity, increased healthcare utilization, and even mortality. The risk of negative outcomes is particularly important for older adults who have increased risk of social isolation. The CARE Center identifies preventable and treatable precursors to social isolation and promotes interventions to optimize quality of life. News story
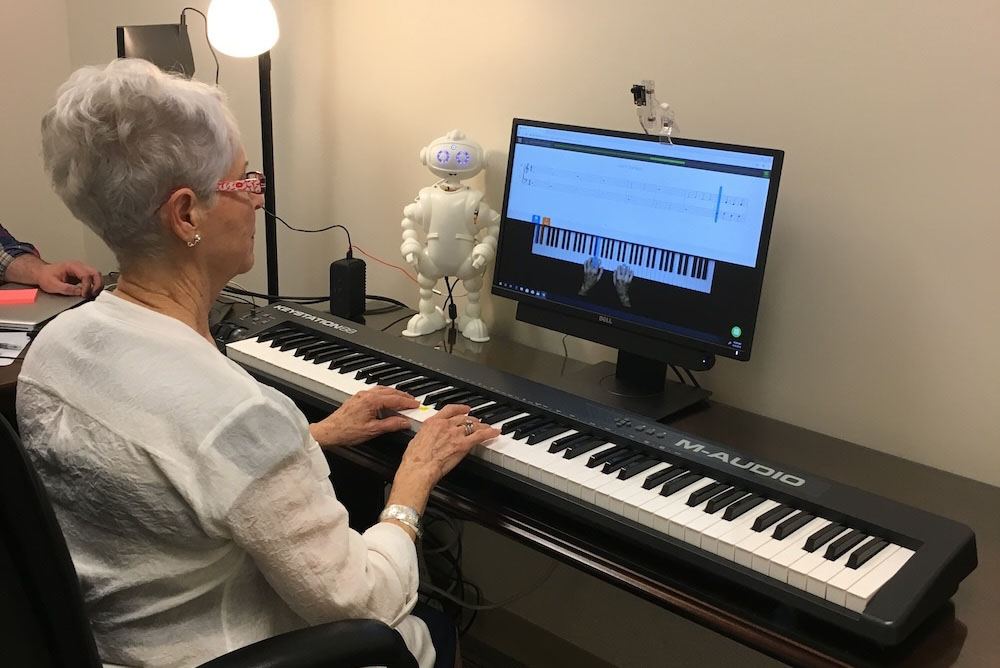
Technology-enabled Cognitive Training
Music learning as cognitive training has been shown to improve memory in older persons at risk for and in early stages of Alzheimer’s disease and related dementias (ADRD). Whether music learning affects all memory processes equally (e.g., verbal memory vs. visual memory) is unknown. In collaboration with Van Robotics, we have conducted a clinical trial exploring the design, development, and feasibility of technology-enabled cognitive training. Our preliminary findings suggest that music learning improves key aspects of memory, but it does not do so uniformly. Understanding how cognitive training affects specific domains of function enables the creation of cognitive training strategies that impact multiple functional domains.

Understanding Physician Barriers to Dementia Diagnosis
Alzheimer’s disease and related dementias are underdiagnosed in rural and medically underserved communities, partly due to lack of access to specialty care. Consequently, primary care and family medicine providers carry the burden of diagnosis and follow-up. The purpose of this study was to identify rurally practicing primary care providers’ perceived barriers to dementia diagnosis and care. Interviews with physicians were conducted. Providers reported being able to identify signs and symptoms of dementias among patients, but reported a reluctance to deliver a diagnosis, for fear of not having resources to manage follow-up care. They also mentioned the high likelihood of stigma affecting how families responded to a diagnosis. Providers reported bottlenecks in specialty care, and a desire to use technology, such as telehealth, to alleviate those bottlenecks. They reported a need for education to close gaps in follow-up care. Our team is in the process of developing a larger-scale survey to understand these barriers.
Undergraduate Research Assistant Applications
Are you an Undergraduate student at the University of Georgia looking to get involved with the CARE Center? Apply to be an Undergraduate Research Assistant!
All research assistants who join our team are required to be enrolled in research for course credit. We ask that students commit at least one year to this position through a research course. Students should be able to commit to their projects, team members and lab. This includes being reliable and accountable, working collaboratively, and producing quality work.
